Dear Valued HMA® Member,
As part of our ongoing commitment to provide you with the best possible customer service and make our program better and easier, we have made some important and beneficial enhancements to the HMA® medical claims payment process. These helpful changes went into effect on October 12, 2023 and will greatly benefit you. We here at Health Matching Account Services, Inc. (HMAS®) are excited to now take the HMA® program to the next level.
We understand that this change is happening very quickly, but we wanted to make this change to benefit you so you wouldn’t have to worry about any more declined transactions or claim reimbursements. As we looked into it, we realized we could make this change very quickly, so we decided to act quickly in the best interests of you, our valued member.
These new enhancements to the HMA® program include:
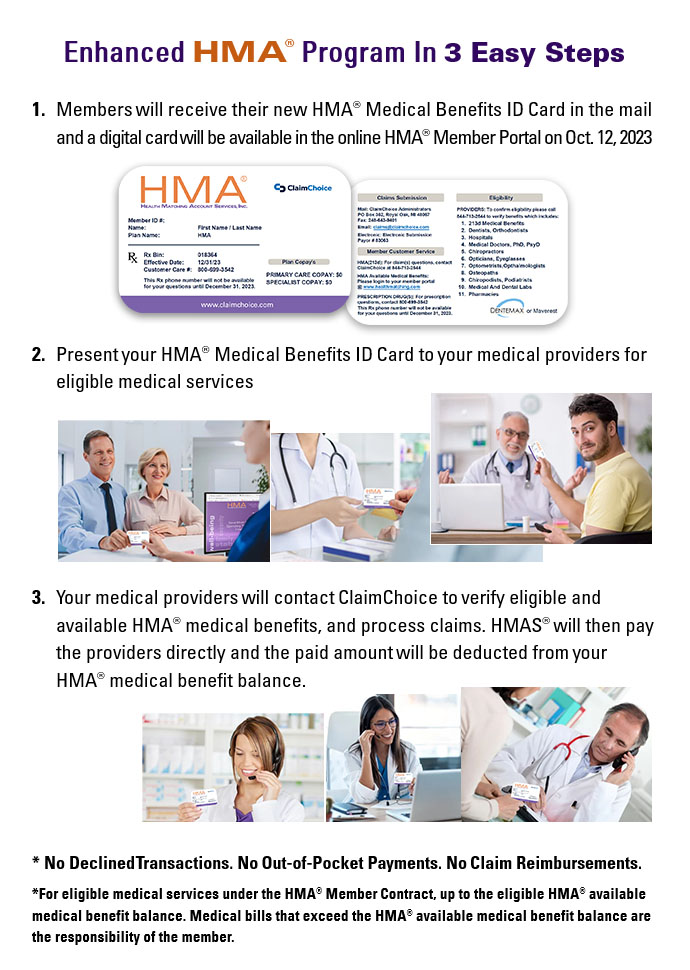
1. Moving Away From Debit Cards: On October 12, 2023, HMAS® introduced our HMA® Medical Benefits ID Card to replace the debit cards. You should have received 2 HMA® Member ID cards in the mail with a letter describing how to use your HMA® ID Card. If you have not received your physical card yet, there is a digital card that will be available in your online HMA® Member Portal.
2. How To Use The HMA® Medical Benefits ID Card: Similar to providing your health insurance card at your medical providers, all you will have to do now is present your HMA® Medical Benefits ID Card to your medical providers at the time of service in order for you to access your HMA® medical benefits.
Your medical providers will then use the Eligibility information on the back of your HMA® Medical Benefits ID card to call ClaimChoice at 844-713-2544 in order to verify your available HMA® medical benefit balance. Please note, the list of covered services has not changed, just the way HMAS® pays claims has changed. HMAS® will work directly with your providers to pay for eligible medical claims, and the billed amount will be deducted from your HMA® medical benefit balance. When the medical provider verifies eligibility, you will not have to pay out of pocket unless you do not have enough available HMA® medical benefits to cover the full amount or it is a non-eligible service under the HMA® Member Contract.
Example 1: You incur a $500 medical bill and have a $1000 available HMA® medical benefit balance. You will present your new HMA® Medical Benefits ID Card to the provider, and the provider will call to verify eligibility. Once the service has been performed, there will be no out of pocket charge to you and HMAS® will pay the provider the $500 to settle the bill, and your available HMA® medical benefit balance will be reduced to $500.
Example 2: You incur a $500 medical bill and have a $200 available HMA® medical benefit balance. You will present your new HMA® Medical Benefits ID Card to the provider, and the provider will call to verify eligibility. The provider will charge you the $300 not covered by the HMA® medical benefit balance, and HMAS® will pay the provider the $200 that is available from the HMA® medical benefit balance, reducing the available benefits to 1 month’s contribution that is required to remain in the HMA® plan at all times in order to keep your plan active with Health Matching Account Services.
3. No More Claim Reimbursements, Debit Card Declined Transactions And White Listing: The old HMA® debit card worked a vast majority of the time when it was swiped, but for certain transactions that were not eligible or coded correctly, HMA® members would experience declined transactions. This would necessitate and result in either the member having to submit the claim online through their member portals for reimbursement after they paid for the claim or the customer calling in to our office for us to potentially white list those providers if it was indeed a qualified medical expense that may have been poorly coded in the payment system of the provider causing the debit card to therefore be declined. Those days are now over thanks to the HMA® Medical Benefits ID Card. No more worries about declined transactions or submitting claim reimbursements within 30 days for eligible medical services!
4. The New HMA® Medical Benefits ID Card Can Be Used At All Types Of Pharmacies, Starting On December 31, 2023: The old HMA® debit card could be used at standalone pharmacies, but not if they were located in grocery stores or online pharmacies. With the new HMA® Medical Benefits ID Card, you will be able to go to over 60,000 pharmacies across the country starting on December 31, 2023. You will present your HMA® Medical Benefits ID Card at the counter of the pharmacy, and the pharmacy will use the Rx BIN# and customer care phone number on the back of the card to verify the amount of eligible HMA® medical benefits you have to complete the transaction. Until the prescription drug card coverage begins on December 31, 2023, you will use the standard HMAS® practices of uploading your prescription claims through your HMA® member portal as a claim reimbursement until December 31, 2023.
The HMA® Medical Benefits ID Cards were mailed out on October 13, 2023. Please be on the lookout for a window envelope with the HMAS® return address. If you have not yet received the physical HMA® Medical Benefits ID Card in the mail and you have a medical appointment, feel free to contact our customer service department at (713) 850-8534. In the mean time, you can access and print off the front and back images of the digital HMA® Medical Benefits ID Card in your online member portal to present to your providers.
To recap, these new enhancements will provide significant advantages to you when receiving medical services. You will no longer have issues with declined debit card transactions or paying out of pocket and submitting claim reimbursements within 30 days, except for pharmacy prescription purchases until December 31, 2023. There will soon be a short video available on your member portal introducing you to the new HMA® Medical Benefits ID Card.
We value your continued trust and partnership. Our objective is to always serve you and we know these changes are the best way to ensure that you receive the most benefit and best experience with the HMAS® program. Thank you for choosing Health Matching Account Services, and we look forward to continuing our meaningful association with you as we work together to transform our industry and change how people think about paying for their medical needs by empowering our members and significantly lowering the cost of health care all across the country.
Many thanks to you, our valued members.
Health Matching Account Services, Inc.